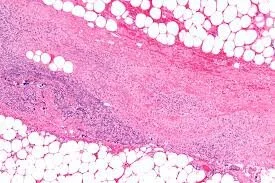
Necrotizing fasciitis is an uncommon, severe infection involving the subcutaneous soft tissues including the superficial fascia. Historically, it has been divided into two types with Type I involving anaerobic flora and Type II involving Streptococcus pyogenes (group A Strep or GAS)—often referred to as “flesh eating bacteria.” Type II can also be associated with other bacteria including staphylococci. The portal of bacterial entry is usually a site of trauma or injury. The most common site of involvement is an extremity. Early differentiation from cellulitis, a less severe skin infection, can be difficult.
A patient with necrotizing fasciitis can present with swelling and induration with some erythema but usually not with defined sharp margins. The area is exquisitely tender. The skin of the infected area can progress rapidly over several days and develop purple or gray discoloration. Over time, pain may be replaced by anesthesia of the infected area.
Necrotizing fasciitis patients commonly have fever and leukocytosis; they often have positive blood cultures. Imaging may reveal gas in the subcutaneous tissue, but this is not always present.
The treatment of necrotizing fasciitis is surgical debridement. In most cases, a large amount of necrotic tissue is removed, commonly parts or entire limbs. Broad-spectrum antibiotics alone are not curative.
Left untreated, necrotizing fasciitis is fatal. Even with treatment, patients may still succumb to the infection. Those that survive have extensive surgical scars and may be permanently disfigured.
Necrotizing fasciitis medical expert witness specialties include infectious disease, vascular surgery, emergency medicine, radiology, microbiology, emergency medicine, urgent care medicine, critical care medicine, pediatric emergency medicine, and forensic pathology.