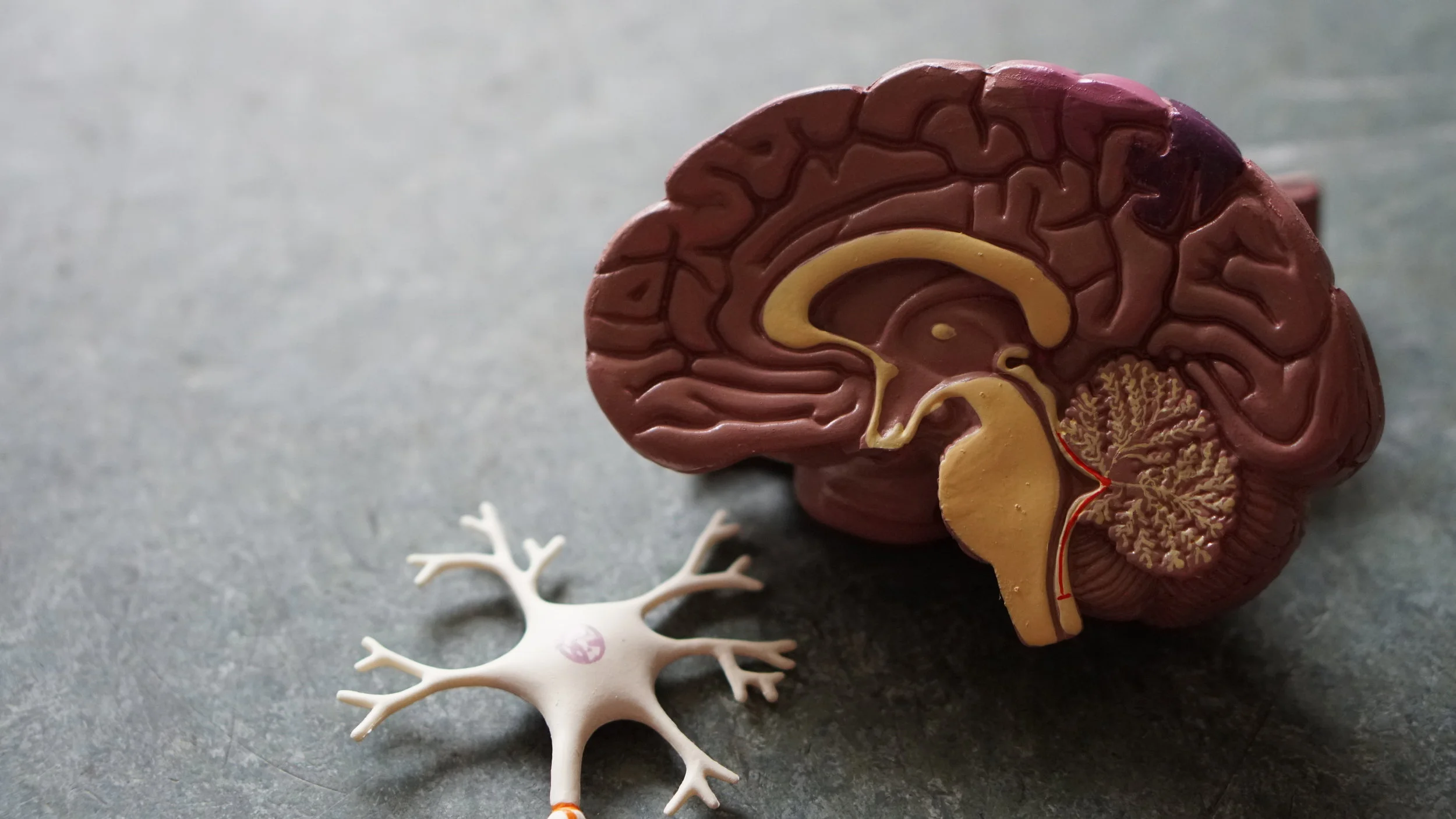
Collections of blood that form in the subdural space in the brain are very common in people 50 years and older, with head trauma and falls being a common cause. The subdural space is the area between the brain surface and the underneath of the skull. Veins carrying blood are in this space and are easily stretched during trauma and can eventually be injured and bleed. It is well-known that subdural blood accumulation will not always be apparent on initial radiologic studies following injury. In fact, it may take up to several weeks for blood to show in this space. The mechanism for this latter scenario involves the veins initially clotting off and then reopening. The delayed bleeding results in blood accumulating, in the days and weeks that follow, and becoming symptomatic. A collection of blood in the subdural space can be very small and not require surgery but when the blood collections in this space is more extensive, it cause brain swelling and edema, and become life-threatening requiring emergency surgery. In some cases of subdural hematoma, the blood not only causes significant mass effect to the brain but also causes secondary brain swelling. Subdural hematomas—especially those with secondary brain swelling—are usually associated with permanent cognitive impairment. The pressure from the additional fluid and swelling permanently damages/destroys the deeper structures leading to permanent brain damage.
Subdural hematoma medical expert witness specialties include neurology, neurosurgery, pathology, forensic pathology, neuropathology, hematology, cardiology, vascular neurology, pediatrics, emergency medicine, pediatric emergency medicine, urgent care, radiology, neuroradiology neurointervention, and biomechanics.