Several characteristics of melanoma have been identified and well-studied. Among the factors studied for primary lesions, the depth of invasion and presence or absence of invasion are most important and are incorporated into the formal American Joint Committee on Cancer (AJCC) staging criteria.
Depth of tumor invasion is the primary criterion for staging, with the presence or absence of ulceration also taken into account. Tumor thickness is measured to the nearest 0.1 mm based on standard Breslow methodology. The deeper the thickness of the tumor, the higher the risk of recurrence, metastasis, and mortality.
Ulceration is defined as the absence of an intact epithelium over the melanoma. Ulceration is an important prognostic factor of the primary tumor in the AJCC staging system in which it is used to define patient subsets for each tumor thickness group. Outcomes in patients with ulcerated primary tumors are worse than in patients with primary melanomas of the same thickness but without ulceration.
A tumor classified as pathologic T1 is defined as a tumor ≤1 mm thick, with T1a being <0.8 mm without ulceration, and T1b being a heterogeneous group including thickness <0.8 mm with ulceration, or 0.8 to 1.0 mm with or without ulceration. T2 is defined as tumors having thickness >1.0 to 2.0 mm and is further subdivided into T2a or T2b based upon the absence or presence of ulceration respectively. T3 is defined as thickness >2.0 to 4.0 mm, which is subdivided into T3a or T3b based upon the absence or presence of ulceration, respectively. T4 is defined as those tumors >4.0 mm in thickness.
The clinical stage grouping then incorporates the pathologic staging into a schema that also includes the presence of lymph node involvement and/or distant metastases. Stage I melanoma is limited to patients with low-risk primary melanomas (T1a, T1b, and T2a) without evidence of regional or distant metastases. Stage I is divided into stages IA and IB based on the thickness of the primary tumor and the presence or absence of ulceration. Stage II disease includes primary tumors that are at higher risk of recurrence (T2b, T3a, T3b, T4a, and T4b) but do not have any evidence of lymphatic disease or distant metastases. Stage II is divided into stage IIA, IIB, and IIC depending upon tumor thickness and the presence or absence of ulceration. Stage III disease includes pathologically documented involvement of regional lymph nodes or the presence of in-transit or satellite metastases. Stage IV disease indicates distant metastasis.
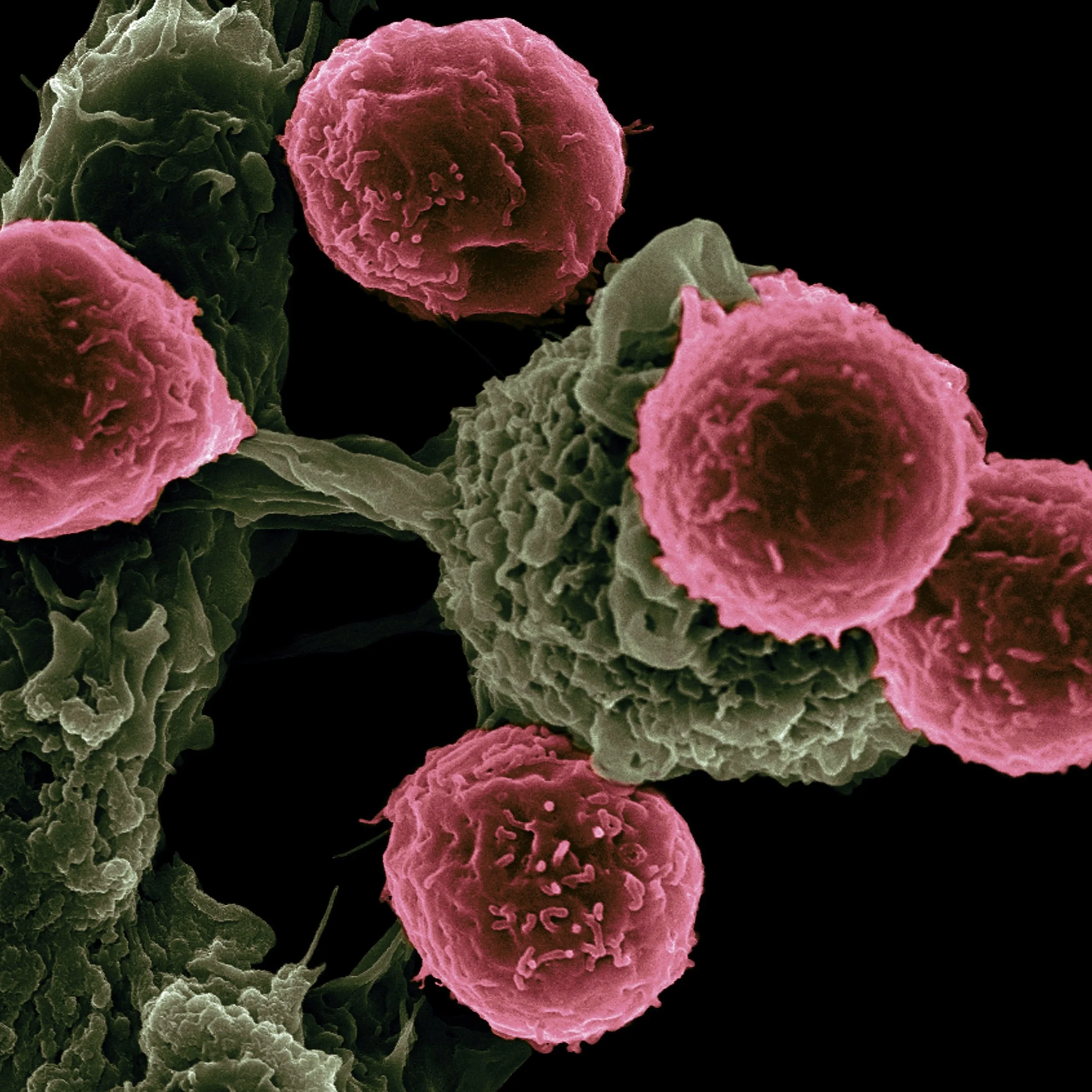
Mitotic rate is a significant prognostic factor within all tumor thickness categories, and it should be assessed and recorded in all primary melanomas. Simply put, the mitotic count indicates the number of cells that are visibly actively dividing as examined under the microscope. Mitotic rate over 4 per mm2 imparts a much higher risk of recurrence, even in thin melanomas.
Other independent factors are less well-studied and, therefore, are not incorporated into the formal staging schema. These adverse factors included the absence of a brisk lymphocytic response and/or absence of regression.
Melanoma staging medical expert witness specialties include oncology, dermatology, dermatopathology, and surgical oncology.