What is hydrocephalus?
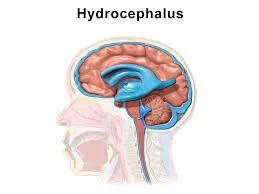
Hydrocephalus is a condition resulting from abnormal accumulation of cerebrospinal fluid (CSF) in the ventricles of the brain. The human brain has four ventricles, which are like chambers. Each ventricle consists of a structure called choroid plexus which produces a clear, colorless fluid called CSF. The CSF coats and protects the brain and the spinal cord. It also contains nutrients that are vital for the nourishment of the brain tissue. As well, the CSF carries waste products away from surrounding tissues.
In normal conditions, CSF circulates in the ventricular system of the brain before being reabsorbed into the blood circulation. Any abnormality in the normal flow of CSF or problems in CSF reabsorption can disrupt the brain and the spinal cord. This disruption of normal CSF flow can also lead to excess build-up of CSF in the brain, which is known as hydrocephalus. An excess of CSF in the brain results in more pressure on the brain tissue which can cause brain damage, decreased brain functionality, and even death.
Who can develop hydrocephalus?
Hydrocephalus can affect individuals of any age group. Most commonly, it is seen in infants and older people. Listed below are important statistics related to hydrocephalus in the United States:
Currently, over 1,000,000 people in the United States live with hydrocephalus
For every 1,000 babies born in the United States, one to two will have hydrocephalus
Hydrocephalus is the most common cause for brain surgery in children
It is estimated that more than 700,000 Americans have normal-pressure hydrocephalus (NPH), but less than 20% receive an appropriate diagnosis
What are the causes of hydrocephalus?
Hydrocephalus can be grouped into congenital and acquired. In congenital hydrocephalus, babies are born with hydrocephalus or develop the condition shortly after delivery. The causes of congenital hydrocephalus are as follows:
Genetic abnormalities that block the flow of CSF
Birth defects in the spinal cord, the spine, or the brain
Complications before birth, e.g., bleeding within the brain ventricles (intraventricular hemorrhage (IVH), subarachnoid hemorrhage, germinal matrix hemorrhage (especially in preterm infants)
Infection during pregnancy, such as rubella infection (which can inflame the fetal brain tissue), meningitis, syphilis, cytomegalovirus, and toxoplasmosis
Trauma to the infant’s head during or following delivery
In infants, intraventricular hemorrhage (IVH) is the most common cause of hydrocephalus. IVH is more common in preterm babies. Conditions that can result in an IVH in preterm and term infants are as follows:
Trauma endured during prolonged labour
Abnormal blood pressure changes
Abnormal fetal presentation, e.g., breech presentation
Hypoxic ischemic encephalopathy (HIE): Brain damage caused by insufficient oxygen and blood supply to the fetal brain tissue
Fetal oxygen deprivation
Head trauma resulting from use of Cytotec or Pitocin to induce labor
Traumatic delivery caused by forceps delivery, macrosomic delivery (large baby), or cephalopelvic disproportion (CPD), i.e., the baby is too large for the size of the mother’s pelvis.
Acquired hydrocephalus can develop at any age and is usually caused by external factors. The causes of acquired hydrocephalus are as follows:
Tumors in the spinal cord or the brain
Central nervous system infection, e.g., bacterial meningitis
Brain injury or stroke
What are the types of hydrocephalus?
Depending on the flow of CSF, hydrocephalus can be divided into two main types: communicating and non-communicating hydrocephalus. In communicating hydrocephalus, the CSF flows normally through the brain ventricles, but cannot flow smoothly outside the brain’s ventricular system due to some obstruction present outside the brain. In non-communicating or obstructive hydrocephalus, the CSF flow is obstructed within the brain’s ventricular system due to an abnormality.
Based on the cause of hydrocephalus, the condition can be divided into two types:
Hydrocephalus ex-vacuo: This type of hydrocephalus results from brain damage caused by stroke or injury. In such cases, the brain tissues around the ventricles shrink. Due to this, the ventricles appear larger than normal. The condition is not a true form of hydrocephalus, but rather ‘pseudo-hydrocephalus.’
Normal Pressure Hydrocephalus (NPH): This type of hydrocephalus can be caused by bleeding in the brain’s CSF (subarachnoid or intraventricular hemorrhage), infection, tumor, head trauma, or can be a complication of surgery. However, many people develop NPH even in the absence of the above causes. In NPH, the increase in cerebrospinal fluid is gradual. Hence, in this type the tissues around the ventricles compensate and the fluid pressure inside the head does not increase. NPH can cause issues with bladder control, walking, and cognitive difficulties (thinking and reasoning). At times, symptoms of NPH can be mistaken for Alzheimer’s disease.
What are the signs and symptoms of hydrocephalus?
Hydrocephalus presents with many signs and symptoms, which vary by the age of the patient and the severity of the condition. Some of the symptoms of hydrocephalus may be seen in other neurologic conditions, hence, accurate diagnosis of the condition is vital for prompt and appropriate treatment.
Hydrocephalus in infants can present with the following signs and symptoms:
Unusually large head
Rapid increase in the size of the head
Bulge on the top of the head
Vomiting
Irritability
Seizures
Eyes fixed downwards (sun setting)
Sucking or feeding issues
Sleepiness
Signs and symptoms in older children, young adults, and middle-aged adults can be as follows:
Nausea and/or vomiting
Blurred or double vision
Headaches
Loss of bladder control and/or frequent urination
Irritability
Sleepiness
Balance problems and coordination issues
Hydrocephalus in the elderly can present as follows:
Progressive mental impairment and dementia
Loss of bladder control and/or frequent urination
Poor coordination and balance issues
Difficulty walking
Decline or slowing of movements
Who diagnoses and treats hydrocephalus?
Specialist doctors who treat hydrocephalus include:
Neurologist
Neurosurgeon
Pediatrician
Neonatologist
How is hydrocephalus diagnosed?
A patient’s signs and symptoms, the neurologic exam, and diagnostic test results are used for the diagnosis of hydrocephalus. A neurologic exam is performed by a specialist to assess the following:
Coordination and balance
Hearing, eye movements, and vision
Muscle strength and reflexes
Mental function and mood
Brain imaging tests are used for the definitive diagnosis of hydrocephalus. These tests may include:
Magnetic resonance imaging (MRI): This test is used to assess the size of the brain ventricles, brain tissue, and CSF flow. It is usually the first test used for diagnosing hydrocephalus in adults.
Computed tomography (CT): This scan is used to check if the brain ventricles are enlarged and if there is an obstruction.
Ultrasound: This test is usually used for diagnosing hydrocephalus in infants and unborn babies, as it is non-invasive and carries no radiation exposure.
Other diagnostic tests:
Lumbar puncture: This test is used to analyse the CSF fluid and assess CSF pressure. CSF is collected via a needle from the lumbar vertebrae of the spinal column.
Intracranial pressure monitoring (ICP): To monitor ICP, a small pressure monitor is inserted into the brain or the ventricles to measure the pressure and detect the amount of swelling. If the pressure is too high, a neurosurgeon may drain the CSF to maintain the flow of oxygenated blood to the brain.
Fundoscopic examination: In this test, a special device is used to view the optic nerve at the back of the eye. With elevated intracranial pressure, the optic nerve is affected and its presence can indicate hydrocephalus.
What are the current treatments for hydrocephalus?
Surgical treatments: Hydrocephalus can be treated with one of two surgical options:
Shunt: A shunt (tube) is surgically inserted into the brain, which is then connected to a flexible tube placed under the skin to drain the excess fluid into either the chest cavity or the abdomen. The excess fluid is then absorbed by the body.
Endoscopic Third Ventriculostomy (ETV): This method improves the flow of CSF out of the brain. In this surgery, a tiny hole is made at the bottom of the third ventricle and the flow of CSF is diverted to relieve pressure. Sometimes this procedure is performed in conjunction with choroid plexus cauterization which can help decrease the production of CSF. In choroid plexus cauterization, electric current is used to burn the CSF-producing tissue (i.e., the choroid plexus) in the lateral ventricles of the brain, so that it produces less CSF.
Generally, shunt systems function well but they can fail to properly drain CSF when there is mechanical failure or infection. If this happens, CSF can once again build up in the brain leading to hydrocephalus and associated symptoms. In such cases, the clogged shunt system is replaced via surgery to restore drainage of CSF.
Usually, shunts require regular monitoring and timely medical checkups. Shunt malfunction can be dangerous for the patient and may necessitate emergency medical attention.Signs and symptoms of shunt malfunction may include:
Nausea and/or vomiting
Headaches
Sensitivity to light
Seizures
Low-grade fever
Double vision
Sleepiness
Supplemental treatments for hydrocephalus may include:
Occupational and developmental therapies for children
Special education teachers for children with learning disabilities
What is the prognosis of hydrocephalus?
Hydrocephalus is a treatable condition. Early diagnosis and prompt treatment are essential for successful recovery. People with properly treated hydrocephalus can live normal lives. However, lack of appropriate treatment can result in permanent neurologic disabilities or death.
Legal Issues Associated with Hydrocephalus
Again, failure to diagnose a patient who has presented with signs and symptoms indicative of hydrocephalus may result in lifelong cognitive impairment, severe neurologic complications, or death.
Hydrocephalus patients who have a surgically placed shunt may also suffer severe complications if a doctor does not properly monitor it. It is also vital that the doctor promptly addresses any adverse symptoms arising due to shunt malfunction. The shunt system could fail due to different reasons, such as movement of the catheter, infection at the insertion site, or blockage of the catheter. In case of shunt malfunction, there would be relapse of hydrocephalus symptoms.
Hydrocephalus in Infants and Medical Malpractice
Failure to diagnose hydrocephalus prenatally and misdiagnosis of hydrocephalus in infants are common causes of medical negligence cases.
In infants with hydrocephalus, if the excess CSF is not drained promptly, there could be permanent damage to the brain tissue. This damage could be seen as scarring of the brain tissue, white and gray matter damage, and even brain tissue necrosis (death) in severe cases. Permanent brain tissue damage can cause cerebral palsy, lifelong learning disabilities, and developmental delays.
Immediate medical treatment of infants with hydrocephalus is critical for preventing permanent brain damage and life-threatening complications. Once an infant is diagnosed with hydrocephalus, surgical drainage is required via either of the procedures listed below:
Shunt systems: A shunt is comprised of catheters, tubing, a reservoir, and a pressure activated valve. The shunt system is placed in the infant’s skull through a hole. A catheter is then inserted through the hole into one of the lateral ventricles. This catheter is connected to a one-way valve system that opens when the pressure in the ventricles exceeds a certain value. Through this catheter the CSF is drained. As the fluid drains, the pressure within the ventricles decreases, which causes closure of the valve until the pressure increases again. The other end of the shunt system is connected to a catheter which is placed in the infant’s abdominal cavity. The excess CSF that has been transported to the abdominal cavity is reabsorbed into the baby’s circulatory system.
Third ventriculostomy: In this procedure, a surgeon makes a hole (perforation) in the infant’s brain to connect the third ventricle to the subarachnoid space (a space in which the CSF flows). This procedure is sometimes used as the first treatment in certain cases of obstructive hydrocephalus. However, this treatment cannot be used if the infant has communicating hydrocephalus.
IF YOU NEED A Hydrocephalus MEDICAL EXPERT, CALL MEDILEX AT (212) 234-1999.
Image courtesy of BruceBlaus. This file is licensed under the Creative Commons Attribution-Share Alike 4.0 International license.