What is arteriovenous malformation (AVM)?
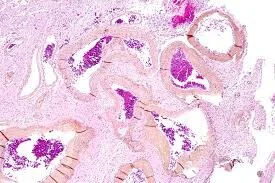
The vascular system of the body consists of the blood vessels--arteries, veins, and capillaries. An arteriovenous malformation (AVM) is a defect of the vascular system in which a vein and an artery communicate with each other via a tangle of blood vessels. The most common cause of an AVM is a defect in the formation of the blood vessels during fetal development, but may also result from trauma, surgery, or disease (e.g., malignancy).
The arteries carry oxygenated blood from the heart to the organs and tissues. The veins carry deoxygenated blood from tissues to the heart.(The exceptions are the pulmonary artery (which carries deoxygenated blood) and pulmonary vein (which carries oxygenated blood) Arteries and veins are normally connected via capillaries. In an AVM, there are no capillaries involved; the arteries and the veins are connected to each other through a tangle of vessels.
The average age when an AVM is detected (particularly for brain AVMs) is mid-30s. A small number of AVMs present at or shortly after birth. Most of them present later in life and can progress during the later years of life.
Where can an AVM occur?
An AVM can occur anywhere in the body. AVMs located in the central nervous system (brain and spinal cord) can be life-threatening if not treated on time.
The direct artery-vein connections in an AVM, termed fistulas or fistulae, have low resistance to blood flow. This results in very high flow rates in those blood vessels leading to and within the AVM. In a brain AVM, these high flow rates can also lower the pressure in the arteries leading to the AVM and to surrounding relatively normal brain tissue. Further, because of the direct A-V connection, the pressure in the artery delivering the blood is transmitted to the vein, that drains the AVM, resulting loss of perfusion to the tissue dependent on that blood supply. This also increases the overall pressure within the vein and can prove dangerous because veins do not operate under arterial pressures.
Arteriovenous Fistula
An arteriovenous fistula (AVF) is an abnormal direct connection between an artery and a vein. Similar to an AVM, an AVF can be congenital but an AVF can also develop after an accident, trauma, or even after a medical procedure. AVFs are created purposely in medicine, for example, for dialysis.
What are the causes of AVM?
The causes of AVM remain unclear. Often, AVM formation is attributed to an abnormality in embryonic or fetal development but there is no direct evidence. No environmental risk factors have been identified for neurological AVM. AVM does not usually have a genetic component, but approximately 5% of AVMs have been found to have an autosomal dominant inheritance of a genetic mutation. The most common genetic mutations include hereditary hemorrhagic telangiectasia or capillary malformation-AVM syndrome.
Important AVM-related statistics are listed below:
AVM affects males and females in equal numbers.
The incidence rate of an AVM is about 1 per 100,000 population per year (about 3000 new cases detected per year in the U.S.)
The population prevalence of an AVM in the United States is about 10 per 100,000, i.e., there are probably about 30,000 individuals in the U.S. who harbor an AVM or have had an AVM that was treated.
What are the signs and symptoms of an AVM?
Symptoms of AVM occur only after a certain amount of damage to the brain or spinal cord has occurred. This can range from minor symptoms such as headache to fatal AVM rupture with hemorrhagic stroke. A small percentage of AVMs are detected incidentally during diagnostic investigation of other medical problems. Such AVMs are usually completely asymptomatic, hence their incidental detection.
AVMs cause reduced oxygen to tissues. The reduced oxygen causes neurological damage through one or more of the following mechanisms:
A change in pressure within the blood vessels
Compression of adjacent neural tissue by the abnormal vascular structures of the AVM
Bleeding (hemorrhage) into surrounding tissues.
Seizures are the presenting symptom in 15-40% of individuals with AVM. Cerebral hemorrhage can occur when an AVM ruptures. In such cases, a large amount of blood is released into the brain. Brain hemorrhage causes the presenting symptoms in about half of the patients with a brain AVM. The risk for cerebral hemorrhage in individuals with AVM is approximately 2-4% per year. The annual rates of brain AVM rupture vary from below 1% to as high as 30%. Headache occurs in 10-50% of those with AVM and may be the presenting symptom.
Other neurological symptoms can occur depending on the location of the AVM. These symptoms may include:
Muscle weakness or paralysis in one area of the body
Loss of coordination (ataxia) sometimes leading to difficulty walking
Difficulty planning tasks (apraxia)
Dizziness
Vision problems
Difficulty speaking or understanding others (aphasia)
Numbness, tingling, or pain
Memory problems and mental confusion
Hallucinations or dementia
Spinal AVMs can present in many ways including sudden and severe back pain that can cause sensory loss, muscle weakness, or localized paralysis, or there can be a more gradual onset of sensation or motor function abnormalities in the extremities.
How is an AVM diagnosed?
Several imaging studies are used to diagnose AVM. Noninvasive imaging technologies that are used to diagnose AVM are computed axial tomography (CT) and magnetic resonance imaging (MRI). CT is particularly useful in identifying a hemorrhage but can identify only large AVMs. MRI is necessary for the initial diagnosis of AVM. Magnetic resonance angiography (MRA) can be used to determine the pattern and speed of blood flow through AVM but can miss small lesions.
Currently, the gold standard for diagnosis of an AVM is x-ray angiography. This test is usually performed by placing a small tube (catheter) in the femoral artery, which is a large artery in the groin. A contrast agent (dye) that highlights blood vessels is injected into the blood vessels that supply the brain, then x-rays can show the structure of blood vessels in and around the AVM. The results of the angiogram help to determine the most appropriate treatment for the patient.
What treatments are currently available for AVM?
No specific medical therapy is currently available for treating an AVM. Medications can be used to control the headaches, pain, or seizures associated with AVM. Surgery may or may not be recommended on a case-by-case basis based on the estimated risks and benefits. Surgery is often necessary because an untreated AVM has a greater risk of hemorrhage.
Three types of surgery are used for AVM, either alone or in combination. These are as follows:
Conventional surgery (microsurgical resection) is used to remove the AVM if the lesion is small and is located in an accessible area that does not involve critically important functional areas.
Endovascular embolization, in which the AVM is blocked off so that blood can no longer flow through it.
Radiosurgery, in which a high dose of radiation is focused on the AVM, which sets off a gradual process that eventually closes the vessels in the lesion.
Sclerotherapy: This method of treatment can be used for AVM outside of the central nervous system. In this method, a liquid medicine called a sclerosant is injected into the AVM to destroy the blood vessels and cause scars to form. The process also leads to less or no blood flow through the AVM.
Who diagnoses and treats an AVM?
Specialist doctors who diagnose and treat an AVM include:
Vascular surgeon
Neurosurgeon
Neurologist
Vascular and interventional radiologist
Vascular neurologist
Medical malpractice and arteriovenous malformation
Negligence in the diagnosis and treatment of an AVM can be life-threatening for the patient. Legal issues associated with the diagnosis and management of an AVM can include the following:
Failure to diagnose an AVM: Although an AVM is a congenital condition, it can remain silent for several decades without any clinical manifestations. However, when a patient presents with signs and symptoms that are indicative of an AVM, it is the responsibility of the doctor to order further investigative tests to diagnose the underlying condition. If the doctor is unsure about the specific diagnosis, he or she should recommend the patient to a specialist. Undiagnosed AVM can lead to serious medical complications and may prove fatal in case of a brain AVM.
Misdiagnosis of an AVM: The presenting symptoms of a brain AVM (headache and seizures) can be non-specific. Other symptoms of an AVM can be observed in other neurologic conditions. If a patient has symptoms suggestive of a brain AVM, the doctor must order specific tests to rule out other diseases and reach a definitive diagnosis. Misdiagnosis of an AVM can be life-threatening, as the patient could be put on wrong medications and or given incorrect treatment.
Medical negligence during surgical treatment of an AVM: Errors in embolization procedure, radiosurgery, or conventional surgery can have adverse consequences.
IF YOU NEED AN Arteriovenous Malformation (AVM) MEDICAL EXPERT, CALL MEDILEX AT (212) 234-1999.